CMS 1500: The Physician Billing Claim Form

In the United States, the billing document, known as the CMS-1500 form, stands out as the focal point when healthcare providers, including physicians, use it to efficiently bill for the services they have rendered. This standard billing document plays a central role in healthcare settings, facilitating seamless communication with insurance companies to guarantee prompt and precise reimbursements. The form, recognized as the CMS-1500, serves as the backbone for processing physician claims, alongside those of other healthcare providers, making it an essential tool in the healthcare industry.
Introducing the CMS-1500 Form as the Healthcare Billing Document for Physicians
Meet the billing document that physicians rely on the most: the CMS-1500 form!
Named after the Centers for Medicare and Medicaid Services (CMS), it holds good importance in the world of healthcare billing in the United States.
Imagine this form as a superhero sidekick for doctors because it’s the primary paper they use to get paid for the essential healthcare services they provide. It’s like a special code that individual providers, group practices, hospitals, clinics, and billing companies all use to ask insurance companies to reimburse them for the care they give to patients.
This amazing CMS-1500 form ensures that doctors, along with other healthcare providers, can communicate with insurance companies in a smooth and organized way. It brings order and consistency to the entire billing process, making sure everyone speaks the same language when it comes to getting paid for healthcare services.
History

The CMS-1500 Claim Form has a history dating back to 1977 when the Health Care Financing Administration (HCFA) was established to manage Medicare and Medicaid.
HCFA introduced the HCFA-1500 form to standardize billing in healthcare. For almost three decades, it was the standard paper claim form for healthcare providers to submit claims for services to Medicare or Medicaid patients, making the process smoother and data consistent.
In 2001, HCFA became the Centers for Medicare & Medicaid Services (CMS), expanding its healthcare roles.
In 2005, the CMS-1500 form replaced the old one, accommodating changes in healthcare practices and regulations. It added new data fields and more diagnostic codes for detailed clinical reporting.
As healthcare moved towards digitization with electronic health records (EHR) and interoperability, the CMS-1500 form was designed for easy electronic data capture and exchange, a significant step in healthcare’s digital transformation.
The Ideal Billing Document for Physicians
The CMS-1500 form is the ideal document for physicians seeking seamless reimbursement for their services in healthcare billing. This form serves as a vital channel of communication between healthcare providers and insurance companies, streamlining the billing process and ensuring timely payments for the valuable care they provide.
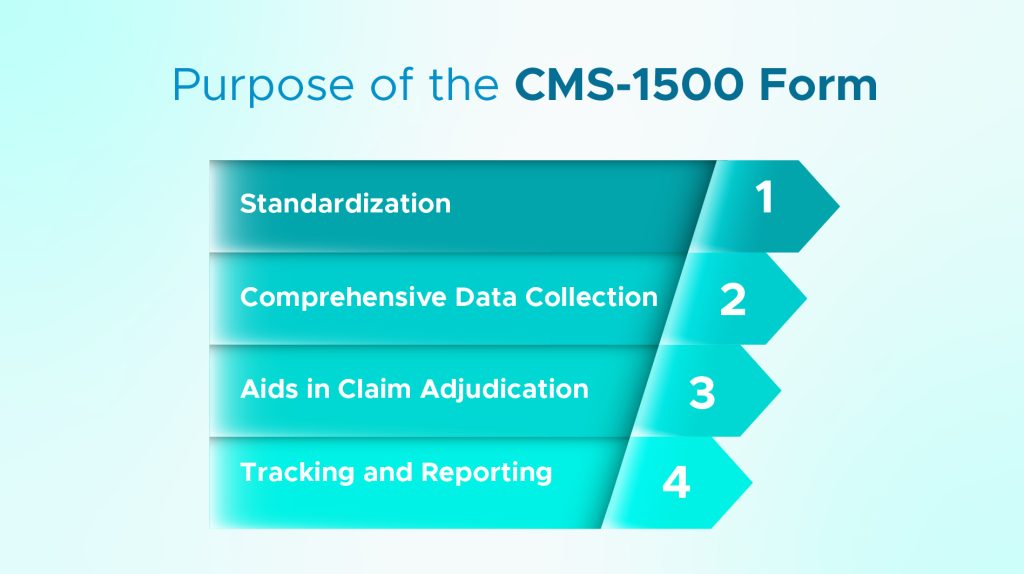
Standardization for Effortless Billing
The CMS-1500 form was created to standardize the complex healthcare billing process. With a universally recognized structure, physicians can now easily navigate the billing process, ensuring accuracy and consistency in their claims. This standardization leads to a greater understanding among all stakeholders, resulting in smoother interactions with insurance companies.
Comprehensive Data Collection for Complete Documentation
The CMS-1500 form excels in collecting a comprehensive range of information, making it a goldmine for physicians seeking to document their patient care thoroughly. It captures essential patient demographics, diagnoses, procedures performed, charges incurred, and provider information, merging all pertinent data into a single, comprehensive form. As a result, physicians can confidently present a detailed account of their services, leaving no room for confusion during the reimbursement process.
Seamless Claim Adjudication for Swift Payments
The CMS-1500 form is essential for quick and accurate claim adjudication in the field of reimbursement. Insurance companies can efficiently validate claims and expedite the payment process for physicians by using its detailed information. Physicians can be confident that their claims will be justified and that they will receive timely and appropriate reimbursement for their essential healthcare services by providing all necessary data in a standardized format.
An Instrument for Tracking and Reporting
The CMS-1500 form serves a broader purpose in the healthcare system beyond its immediate billing function. It provides a valuable record of services rendered, which is invaluable for tracking, reporting, and analysis. This data can ultimately inform healthcare policy, planning, and research. Physicians can contribute to the advancement of healthcare practices by generating valuable insights through the data collected on the CMS-1500 form.
Usage in Healthcare Field
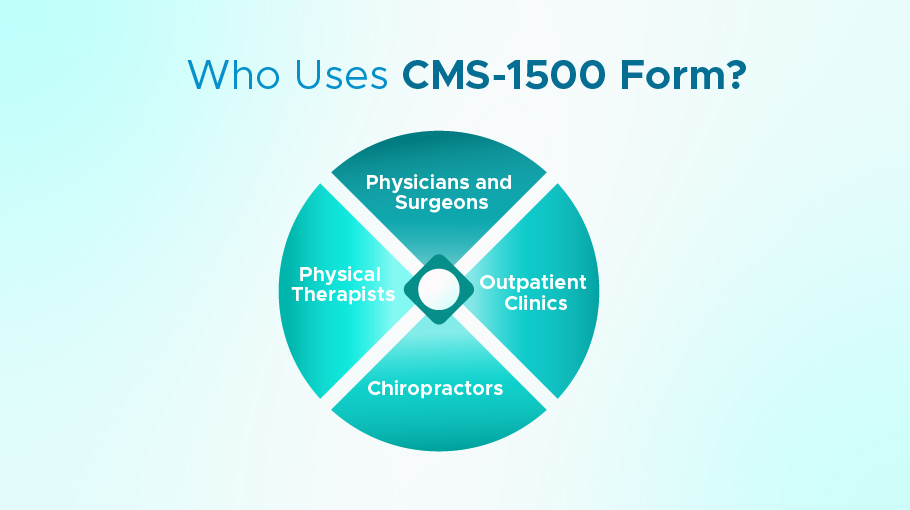
An extensive range of healthcare providers uses the CMS-1500 form, which includes:
Physicians and Surgeons
Doctors use the CMS-1500 form to bill for professional services, ranging from consultations and evaluations to surgeries and post-operative care.
Physical Therapists
Therapists use the form to bill for therapeutic services, including patient evaluations, treatments, and related supplies.
Chiropractors
Chiropractors use the CMS-1500 to bill for their services, including spinal adjustments, physical modalities, and other chiropractic treatments.
Outpatient Clinics
Clinics use the form to bill for various outpatient services, such as preventive care, minor surgeries, and diagnostics.
Healthcare providers use CMS-1500 to get accurate, timely reimbursements from insurers. Its standardized format makes it easier for both providers and insurers to submit and process claims.
On the other hand…
the CMS-1500 form benefits insurance companies and healthcare providers by providing a standardized format for claims. This reduces errors, facilitates processing, and ensures payments are justified.

